Understanding Acute Rhinosinusitis
Acute rhinosinusitis occurs when the lining of the inside of the nose and the sinuses become irritated and swollen. It is also called sinusitis, or a sinus infection.
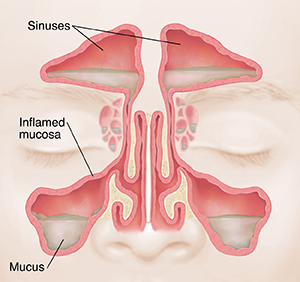
Sinuses are air-filled spaces in the skull behind the face. They help to filter out pollutants, microorganisms, dust, and other irritants. Adults have 4 paired sinus cavities. They are kept moist and clean by a lining of mucosa. Things such as pollen, smoke, and chemical fumes can irritate the mucosa. It can then swell up. As a response to irritation, the mucosa makes more mucus and other fluids. Tiny, hairlike cilia cover the mucosa. Cilia help carry mucus toward the opening of the sinus. Too much mucus may cause the cilia to stop working. This blocks the sinus opening. A buildup of fluid in the sinuses then causes pain and pressure.
Bacteria can become trapped in this fluid leading to an infection.
What causes acute rhinosinusitis?
Rhinosinusitis can result from viral, bacterial, or fungal infections. Viral is the most common cause. You are more likely to get an infection after having a cold or the flu. In some cases, a sinus infection can be caused by bacteria. Although rare, fungal infections can also be the cause, particularly in people with weak immune systems.
You are at higher risk for a sinus infection if you:
-
Are older in age
-
Have structural problems with your sinuses such as
-
Nasal polyps which are growths on the lining of the nose or sinuses,
-
A deviated septum- when the bone and cartilage that separates the 2 nasal passages is crooked
-
A nasal bone spur or growth
-
A narrowing of the sinus openings
-
Smoke cigarettes or are exposed to secondhand smoke
-
Are exposed to changes in pressure, such as from flying a lot or deep-sea diving
-
Have asthma or seasonal allergies
-
Have a weak immune system or taking medicines that suppress your immune symptom
-
Have dental disease
-
Are regularly exposed to air pollution
Symptoms of acute rhinosinusitis
Symptoms of acute rhinosinusitis often last around 7 to 10 days. If you have a bacterial infection, they may last longer. They may also get better but then worsen. You may have:
-
Runny or stuffy nose
-
Face pain or pressure under the eyes and around the nose
-
Headache
-
Fluid draining in the back of the throat (postnasal drip)
-
Congestion
-
Nasal drainage that is thick and colored (often green) instead of clear
-
Cough
-
Problems with your sense of smell
-
Ear pain or hearing problems
-
Fever
-
Tooth pain
-
Fatigue
-
Bad breath
Diagnosing acute rhinosinusitis
Your healthcare provider will ask about your symptoms and past health. They will look at your ears, nose, throat, and sinuses. Imaging tests, such as X-rays, are often not needed.
It can be hard to figure out if a sinus infection is caused by a virus or bacterium. Your healthcare provider may take a sample of mucus from your nose to check for bacteria.
Treating acute rhinosinusitis
Most sinus infections will go away within 10 days. Your body will fight off the virus.
Role of antibiotics:
-
Viral illnesses typically resolve after 3 to 5 days and do not require antibiotics.
-
Using antibiotics to treat viral infections can lead to unnecessary side effects ranging from mild rash to severe allergic reactions, antibiotic-resistant infections, and C. diff infection (diarrhea, colon damage and even death).
-
However, for some sinus infections, your healthcare provider might recommend "watchful waiting" or "delayed antibiotic prescribing." Talk to your healthcare provider about the best treatment for your illness.
You may have a bacterial infection instead if.
-
Your symptoms persist beyond 10 days
-
After an initial period of improvement, your symptoms worsen
-
You have high fever 100.4°F (38°C) or higher with nasal discharge and facial pain
Your healthcare provider will then give you antibiotics. Take this medicine until it is gone, even if you feel better.
To help ease your symptoms, your healthcare provider may advise:
-
Over-the-counter pain relievers. Medicines such as acetaminophen or ibuprofen can ease sinus pain. They may also lower a fever. Carefully read and follow instructions on over-the-counter medicine product labels before taking them. Do not take these types of medicines if you have kidney or liver disease unless instructed by your doctor.
-
Nasal washes. Washing your nasal passages with salt water may ease pain and pressure. It can rinse out mucous and other irritants from your sinuses. Your healthcare provider can show you how to do it.
-
Nasal steroid spray. This prescription medicine can reduce inflammation in your sinuses. Intranasal steroids may help by reducing swelling, which can help relieve the obstruction.
-
Other medicines. Decongestants, antihistamines, and other nasal sprays may give short-term relief. They may help with congestion. Talk with your healthcare provider before taking these medicines, especially antihistamines. These are generally used only when there is a diagnosed allergy.
Preventing acute rhinosinusitis
You can help prevent a sinus infection with these steps:
-
Wash your hands well and often.
-
Look at your local air quality index if air quality puts you at risk. The index will help you limit how much air pollution you're around .
-
Stay away from people who have a cold or upper respiratory infection.
-
Don't smoke. And stay away from secondhand smoke.
-
Use a humidifier to moisten the air at home and be sure to keep it clean.
-
Make sure you are up-to-date on your vaccines, such as the flu shot, COVID vaccine, and pneumococcal vaccine.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Pain that gets worse
-
Symptoms that don’t get better, or get worse. You have a severe headache that does not get better when you use pain medicine.
-
New symptoms appear such as:
-
Pain or swelling around your eyes, difficulty in moving your eyes, severe pain when you do, changes in vision
Call 911
Call 911 or get immediate medical care if you have:
-
Neck pain or stiffness in the neck along with high fever
-
Confusion, disorientation, extreme lethargy, other mental changes, or feel like you are going to pass out.