When Your Child Needs Bladder Reconstruction Surgery
Your child is having bladder surgery. You may feel scared for your child and have many questions. This is normal. Learn what to expect with the surgery and discuss any questions or concerns you may have with your child’s doctor.
Why is bladder reconstruction surgery needed?
Your child's doctor advises surgery to fix your child’s bladder because it isn’t working correctly. During the surgery, the bladder may be patched or rebuilt. In some cases, a new opening (stoma) is made for urine to travel out of the body.
How should we get ready for this surgery?
-
Tell your child's doctor about any medicines your child takes. Include vitamins, herbs, supplements, and both over-the-counter and prescription medicines. You may need to have your child stop taking certain medicines, such as ibuprofen, before the surgery.
-
Tell the doctor about any allergies and health problems your child has. Before the surgery, your doctor will:
-
Take your child's temperature, weight, and height.
-
Do a physical exam of your child.
-
Ask about any recent illnesses, such as sore throat, fever, or colds.
-
Explain the type of surgery, the expected outcomes, complications, postop care, home care, and follow-up visits. Be sure to have all your questions answered.
-
Follow any directions your child is given for not eating or drinking before surgery. This includes any directions for bowel prep. If you don't follow the instructions, the surgery may have to be delayed.
-
Meet with your child’s anesthesiologist before the surgery. They give your child medicine (general anesthesia) so your child sleeps and does not feel pain during the surgery. They will ask questions about your child's allergies, medicines your child takes, and past history or a family history of any bad reactions to anesthesia. The anesthesiologist also closely watches your child’s heart rate, blood pressure, and oxygen levels during the procedure.
-
You will have to sign consent forms for your child's surgery.
What happens before the surgery?
Your first concern is to make your child feel safe and secure. You can bring your child's comfort toy to help your child relax. Assure your child that you will see them as soon as the surgery is over. Your child will be given a mild sedative to relax. When it’s time for the procedure, your child will be given medicine to sleep through the surgery (general anesthesia). A soft plastic tube (catheter) may be put into the bladder to drain urine during and after surgery.
What happens during the surgery?
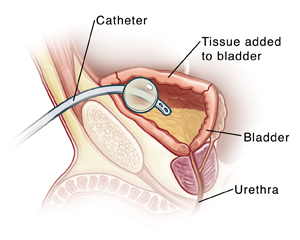 |
| A catheter will be used to help drain urine during and after the surgery. In some cases, the catheter may be passed through an opening made in the abdomen. |
One or more of the following may be done:
-
The bladder may be made larger (augmented). This can be done with tissue from another part of the body.
-
The new bladder can drain through the tube that carries urine out of the body (the urethra). Or the new bladder may be drained through a stoma made in the belly (abdomen). A stoma is a new opening for urine to leave the body. To drain urine, a catheter can be put into the stoma and removed each time the bladder needs to be emptied.
What happens after the surgery?
You will be able to see your child soon after surgery. Nurses will care for and closely watch your child as they begin to wake up from the anesthesia. After waking up, your child may cry and act confused. This is common. Medicine may be given to ease any pain. The catheter that was put in place during the surgery will stay in place for about 3 weeks. You will be given detailed care instructions for the catheter.
Recovering from the surgery
Your child may need to stay in the hospital for 4 to 10 days. The doctor will tell you when your child is ready to leave the hospital. If your child had a stoma placed, a provider will teach you how the stoma is used and how to care for it. As your child heals, the stoma will be checked for problems.
Follow-up care
Before your child leaves the hospital, you will be given instructions for giving care at home. Follow these carefully. Make a follow-up appointment with your child’s doctor within the next 1 to 2 weeks. Your child’s recovery and future care will be discussed during the appointment.
When to contact your child's doctor
Contact your child’s doctor right away if:
-
Your child has a fever of 100.4ºF (38°C) or above, or as directed by your doctor.
-
Your child has chills.
-
Your child's i incision site is red, swollen, draining, or bleeding.
-
Your child's tube is not draining or falls out.
-
Your child has severe belly pain or bloating.
-
Your child has nausea or vomiting.
-
Your child's appetite is poor.
-
Your child's pain doesn’t get better or gets worse
-
You have trouble with your child's stoma.
-
There is blood in the catheter or urine.
How to take a child’s temperature
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The doctor may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The doctor may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the doctor what type to use instead. When you talk with any doctor about your child’s fever, tell them which type you used.
How can I help my child get ready for surgery?
Many hospitals have staff trained in helping children cope with their hospital experience. This person is often a child life specialist. Ask your child’s doctor for more information about this service. There are also things you can do to help your child prepare for the procedure. The best way to do this depends on your child’s needs. Start with the tips below:
-
Use brief and simple terms to describe the procedure to your child and why it’s being done. Younger children tend to have a short attention span, so do this shortly before the surgery. Older children can be given more time to understand the procedure in advance.
-
Make sure your child understands which body parts will be affected in the procedure.
-
As best you can, describe how receiving anesthesia will feel. For instance, the medicine may be given as gas that comes out of a mask. The gas may smell like bubble gum or another flavor. It will make your child sleepy so they nap during the procedure.
-
Tell your child what they will likely see in the operating room during the surgery. For instance, you could tell them who will be there or that the person giving your child medicine to help your child nap will be in uniform.
-
Allow your child to ask questions and answer these questions truthfully. Your child may feel nervous or afraid. They may cry. Let your child know that you’ll be nearby during the procedure.
-
Use play, if appropriate. With younger children, this can include role-playing with a child’s favorite toy or object. With older children, it may help to read books about what happens during the procedure.
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Vinita Wadhawan Researcher
Date Last Reviewed:
5/1/2025
© 2000-2026 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.