For Kids: Taking Your Insulin
The digestive system breaks down food, resulting in a sugar called glucose. Some of this glucose is stored in the liver. But most of it enters the bloodstream and travels to the cells to be used as fuel. Glucose needs the help of the hormone insulin to enter the cells. Insulin is made in the pancreas, an organ in the abdomen (belly). The insulin is released into the bloodstream in response to the presence of glucose in the blood.
Think of insulin as a key. When insulin reaches a cell, it attaches to the cell wall. This signals the cell to create an opening that allows glucose to enter the cell. Without insulin, your cells can’t get glucose to burn for energy. This is why you may feel weak or tired.
The insulin you are missing can be replaced with shots of insulin (injections). Some kids also use insulin pumps. Then your body can burn glucose for energy. This helps keep your blood sugar within a healthy range.
Feeling nervous is normal
Most people with diabetes are scared to give themselves insulin injections at first. Even your parents were probably nervous giving you your first injections. But after a while, it became much easier. With a little practice, you’ll get used to injections, too. And pretty soon you won’t feel nervous or scared.
Types of insulin
The types of insulin are:
-
Fast-acting insulin. Take fast-acting insulin with meals. You have to eat within 15 minutes of taking it.
-
Regular or short-acting insulin. Short-acting insulin is also usually taken before a meal. It will usually reach the bloodstream within 30 minutes after injection.
-
Intermediate-acting insulin. Intermediate-acting insulin takes longer to start working than fast-acting insulin. But it stays in your bloodstream longer.
-
Long-acting insulin. Long-acting insulin makes sure there is a little insulin in your bloodstream at all times. It helps keep your blood sugar in control. These shots can last the whole day.
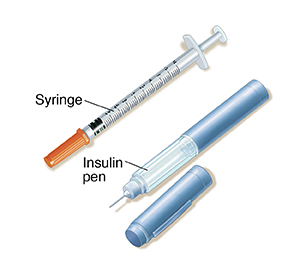
Using a syringe
Always test your blood sugar before injecting insulin. Blood sugar readings help you decide how much insulin to give yourself. When injecting insulin, make sure you inject into the fat just under the skin. Many people with diabetes inject using a syringe.
Ask your doctor to teach you how to rotate your injection site. Also ask how to prevent injecting into areas of lipohypertrophy. This is a bump under the skin caused by injecting insulin in the same spot many times. Also ask about how to inject insulin correctly and how to prevent injecting insulin into the muscle. This is to make sure insulin is absorbed in the correct way.
Follow the steps below for injecting insulin with a syringe.
Step 1: Getting ready
-
Gather your supplies. Here’s what you’ll need:
-
A new syringe
-
Insulin
-
Alcohol wipes
-
Special container to throw out the old needle (sharps container). This can be bought at a drugstore or medical supply store. Or you can use any puncture-proof container with a puncture-proof lid, like an empty laundry detergent bottle.
-
Parent, teacher, or another adult to watch
-
Wash your hands. Use soap and warm water.
-
Clean the insulin bottle. Wipe the top of the rubber top (stopper) of the insulin bottle (vial) with an alcohol wipe.
-
Prepare the insulin. If you use cloudy insulin, roll the bottle gently between your hands about 20 times. Don’t shake the insulin. And don’t use cold insulin. Instead, keep 1 bottle at room temperature and put the rest in the refrigerator.
Step 2: Preparing the syringe
-
Remove the syringe from its package.
-
Take the cap off the needle.
-
Draw air into the syringe. Pull back the plunger to get air into the syringe. Pull the plunger back to the mark (line) for the number of units of insulin you want to inject. The mark on the syringe nearest the needle is 0 (not 1).
-
Inject air into the insulin. Hold the bottle on a flat surface with 1 hand. With your other hand, hold the syringe straight up and down. Slowly push in the plunger to inject air into the insulin.
-
Turn bottle with the syringe upside down. Keep the needle in the stopper. Flip the syringe and bottle so that the bottle is now on top, and the syringe is on the bottom. Be careful not to bend the needle when tipping the insulin bottle.
-
Draw insulin into the syringe. Keep the tip of the needle below the level of insulin. You may need to pull the needle out a little. Slowly pull back the plunger to draw out insulin. Ask an adult to check the dose.
-
Check for air bubbles. Gently tap the syringe while the needle is still in the stopper. The air bubbles will move to the top of the syringe. Push the plunger in a tiny bit to release the air bubbles back into the insulin bottle. Your doctor, nurse, or a diabetes educator may show you other ways to remove air bubbles.
-
Remove the needle from the insulin bottle.
Step 3: Giving the injection
-
Clean the injection site. Use an alcohol wipe to clean the area where you’re going to inject. Let the area air-dry. If the skin is wet with alcohol, the injection will sting.
-
Pinch an inch of skin. Pull up about 1 inch of skin. Pinch the skin gently. Don’t squeeze it. This is to make sure you don’t inject into a muscle.
-
Insert the needle. Insert the needle into the skin at the angle you were shown. Push the needle in until you can’t see it anymore.
-
Inject the insulin. Slowly push in the plunger until the syringe is empty.
Step 4: Removing the needle
-
Count to 5 before pulling out the needle.
-
Remove the needle from the skin.
-
Watch the injection site for leaking insulin and for bleeding. If the site bleeds, dab it with a cotton ball or tissue. If insulin leaks, ask your doctor, nurse, or diabetes educator to make sure you are doing it correctly.
Step 5: After the injection
Using an insulin pen
You can also use injection pens to get the insulin you need. Injection pens look like writing pens. Insulin pens hold cartridges of insulin. A new needle is used for every injection. There are different kinds of insulin pens. Your doctor, nurse, or diabetes educator will tell you which pen is best for you. One of them will also show you how to use the pen. Smart pens are also called connected insulin pens. These pens can be programmed to calculate insulin doses. They send the information to your smartphone.
Tips for pen users
-
Wash your hands with soap and water.
-
Clean the injection site with an alcohol wipe.
-
Use a new needle each time.
-
Never leave the needle on the pen when you’re not using it.
-
Before injecting, tap the needle with your fingertip to get rid of air bubbles.
-
Then test the pen by dialing to 2, pressing the injection button all the way. Insulin should come out of the needle when you do this. If not, check for air bubbles again. Then test again. If no insulin comes out after 3 tries, start over with a new needle. It may also be time to change the cartridge with insulin.
-
Ask an adult to check the insulin dose you have dialed for yourself.
-
There are different types of pen needles. Know what type you are using and how to use it.
-
Standard pen needle. This needle often has a removable outer and inner cover. Both covers need to be removed before the injection.
-
Safety pen needle. This needle has a removable outer cover. The inner cover is a fixed safety shield that is not removed. Instead, the shield will be pushed back. This will expose the needle as the injector is pressed against the injection site.
-
When you get a new box of needles, always check to see what kind of needle it is. It might be different from what you are used to. If you are not sure how to use the new needles, talk with your doctor.
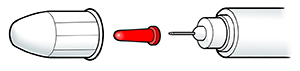 |
| Standard pen needle. |
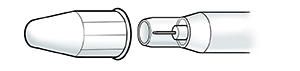 |
| Safety pen needle. |
Storing insulin
-
Keep insulin you are not using in the refrigerator. Make sure it is never frozen.
-
Use insulin before it goes bad (expires). For pen users, the expiration date is usually on the box.
-
Use insulin within 28 days of opening it.
-
Carry your insulin in a bag made to protect it from heat and cold.
Injection spot
It's up to you to find the best spot (site) to inject insulin. When choosing a site, keep these facts in mind:
-
You can inject insulin in the back of your arms, buttocks, the top or sides of your thighs, and your belly (abdomen). Stay at least 2 inches away from the bellybutton (navel).
-
Insulin works fastest when injected into the belly.
-
You need to change injection sites often. Leave about 1 inch between injection sites.
Giving yourself injections
You don't have to give yourself injections until you are ready. Tell your parents or your doctor, nurse, or diabetes educator how you're feeling. They will support you and help you. And, when you do decide to start giving yourself insulin, they will continue to help you.
To learn more
Still have questions about diabetes? Try these websites: