Understanding Gastric Ulcers
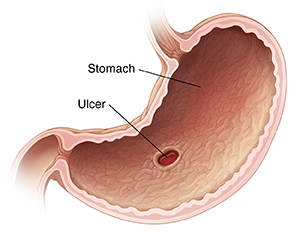
A gastric ulcer is an open sore in the stomach lining. It's sometimes called a peptic ulcer. This is a more general term for ulcers that may be in the stomach or the upper part of the small intestine. Ulcers can cause pain. But they may also have no symptoms for a long time.
What causes gastric ulcers?
Gastric ulcers have a few common causes. To find the cause of your ulcer, your health care provider will give you an exam and take your health history. They may also order some tests. The main causes of gastric ulcers include:
-
Infection with the H. pylori (Helicobacter pylori) bacteria. This damages the stomach lining. Digestive juices can then harm the digestive tract.
-
Long-term use of some over-the-counter pain medicines, such as nonsteroidal anti-inflammatory drugs (NSAIDs). These include ibuprofen, naproxen, and aspirin. This reduces the body’s ability to protect the stomach from damage.
Other causes of gastric ulcers include:
-
Smoking cigarettes.
-
Radiation therapy.
-
Stomach cancer.
-
Zollinger Ellison syndrome.
-
A family history of ulcers.
-
A tumor in the digestive tract (rare).
Symptoms of a gastric ulcer
Ulcer symptoms may appear and then go away for a time. Symptoms of a gastric ulcer may include:
-
Stomach pain. This is often a dull or burning feeling toward the top of your belly. Eating spicy food and drinking alcohol can make it worse.
-
Feeling full or bloated.
-
Heartburn or acid reflux.
-
Upset stomach (nausea) or vomiting.
-
Vomiting blood.
-
Lack of appetite.
-
Weight loss.
-
Black stool.
-
Red blood in the stool.
Treatment for a gastric ulcer
Treatment for gastric ulcers may depend on what is causing them. Treatment may include:
-
Not using NSAIDs. You will likely need to stop taking these medicines. But in some cases, these medicines can’t be safely stopped. Check with your health care provider to see what is best for you before stopping any medicines.
-
Taking medicines to ease symptoms. These medicines may help to reduce the amount of acid your stomach makes. They also may help coat your stomach lining. These include:
-
H2-blockers (histamine receptor blockers). These reduce the amount of acid your stomach makes by blocking the hormone histamine. Histamine helps to make acid.
-
Proton pump inhibitors. These lower stomach acid levels and protect the lining of your stomach and duodenum (the first part of the small intestine).
-
Mucosal protective medicines. These protect the stomach's mucus lining from acid damage so it can heal.
-
Antacids. These quickly weaken or neutralize stomach acid to ease your symptoms.
-
Taking antibiotics. If your ulcer was caused by H. pylori bacteria, your provider will likely prescribe antibiotics to get rid of the infection. It may take 8 to 12 weeks of medicine to relieve symptoms and heal the ulcer. Take all of the antibiotics as prescribed. Not taking all of the antibiotics can keep the bacteria in your system.
-
Having an endoscopy. This is often done to check the stomach and diagnose the ulcer. In some cases, it can also treat the ulcer and help stop bleeding in actively bleeding ulcers. It involves passing a flexible tube through your mouth into your stomach and small intestine.
-
Having surgery. You may need this if there are complications from the ulcer, such as perforation (hole) or obstruction (blockage).
Making some lifestyle changes can reduce ulcer symptoms. It may also prevent more damage to your digestive tract. These changes include:
-
Not taking over-the-counter pain medicines, such as NSAIDs. Talk with your provider about using another type of pain reliever.
-
Not taking aspirin unless your provider has advised it.
-
Limiting the amount of alcohol you drink.
-
Quitting smoking.
Possible complications of a gastric ulcer
Gastric ulcers can have serious complications. These can include:
An ongoing infection with H. pylori may be a risk factor for stomach cancer. This is why it's important to get rid of these bacteria.
When to contact your doctor
Contact your health care provider right away if you have any of these:
-
Vomiting blood, or vomit that looks like coffee grounds
-
Bloody, black, or tarry-looking stools
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
-
Chills
-
Pain that gets worse
-
Symptoms that don’t get better with treatment, or symptoms that get worse
-
New symptoms
Online Medical Reviewer:
Daphne Pierce-Smith RN MSN
Online Medical Reviewer:
Lalitha Kadali
Online Medical Reviewer:
Melinda Murray Ratini DO
Date Last Reviewed:
3/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.